Question 1: Glutathione consists of which of the following amino acids?
A. Glutamate, cysteine, Lysine
B. Tryptophan, Glycine, Isoleucine
C. Glutamate, Cysteine, Glycine
D. Glutamate, Tryptophan, Arginine
E. Tryptophan, Valine, Arginine
Click to see the answer
Answer: C
Glutathione is a naturally occurring tripeptide produced by the liver. Glutathione is an antioxidant that prevents oxidation of hemoglobin to methemoglobin.
G6PD (Glucose-6-phosphate dehydrogenase) enzyme is required to generate NADPH. This NADPH is utilized to keep glutathione in reduced form (GSH). This GSH prevents the oxidation of Hemoglobin. Deficiency of G6PD enzyme causes hemolytic anemia.
Diagnosis of G6PD deficiency is done by Spectrophotometric assay. Coomb’s test is done to distinguish if the lysis of RBCs is due to G6PD deficiency or an autoimmune disorder. Hence Coomb’s test is considered as the differential diagnosis test.
Question 2: JT is a 29-year-old female who is taking Oxcarbazepine BID for epilepsy. She came to the pharmacy to seek some recommendations on Oral Contraceptives. What would be the pharmacist’s concern?
A. Oxcarbazepine does not have a significant effect on the pharmacological action of oral contraceptives and can be given.
B. Oxcarbazepine is a metabolite of carbamazepine which signifcantly reduces the efficacy of combined contraceptive pills.
C. Ask the doctor to change Oxcarbazepine to carbamazepine to avoid any interaction.
D. No need for contraceptives as Oxcarbazepine reduces ovulation.
E. Reduce the dose of contraceptives as Oxcarbazepine increases the efficacy of contraceptives.
Question 3: Where is Testosterone produced in the body?
A. Seminiferous tubules in testes in men.
B. Leydig cells in men and ovaries in women
C. Testosterone is a male sexual hormone and is produced only in epidydimis in the testes of men.
D. Adrenal gland is the primary source in men and ovaries in women.
E. Testosterone is produced by parathyroid gland in both men and women.
Click to see the answer
Answer: B
Testosterone is produced by Leyding cells in the testes in men and ovaries in women. Adrenal glands also produce testosterone but in very small quantity in both men and women.
Also remember: Sperms are produced by seminiferous tubules and mature in the epididymis. Seminal fluid is produced from seminal vesicles.
Question 4: Fluoride toxicity and Stannous fluoride toxicity of fluoride is 8 mg/kg. The weight of the patient is 22 lb. If 0.4% stannous fluoride is used how much minimum dose is required to cause toxicity? (4.1 mg of stannous fluoride contains 1 mg of fluoride)
A. 82 ml
B. 8.2 ml
C. 180.4 ml
D. 82000 ml
E. 320 ml
Click to see the answer
Answer: A
Explanation
Step 1: Weight 22 lb = 10 kg.
The toxicity of fluoride is 8 mg/kg. So 8 x 10 = 80 mg.
Step 2: Now, 4.1 mg stannous fluoride – 1 mg of fluoride.
? – 80 mg of fluoride. (Cross multiply)
= 4.1 x 80/1 = 328 mg of stannous fluoride will cause toxicity.
Step 3: 0.4 gm = 400 mg.
400mg of stannous fluoride – 100 ml
328 mg of stannous fluoride – ? = (328 x 100)/400 = 82 ml (Cross multiply)
Question 5: A 7-year-old woman with metastatic breast cancer had a mastectomy and started chemo and radiation, even though she took her antiemetics as prescribed she is having nausea and vomiting 6 to 7 times a day and she came to the pharmacist saying she gets tired and she would rather die than go through this again. Answer the following questions based on the information provided.
Question 5.1: What is the appropriate question to ask her?
A. Are you sure you took your anti emetics as prescribed?
B. What adverse effects were you expecting from your chemo treatment?
C. Do you know how your chemotherapy works?
D. When is your next scheduled check up?
E. How do you know it is because of chemotherapy?
Click to see the answer
Answer: A
Explanation: Here the patient is complaining about the symptoms. So a pharmacist has to make sure that the person took her medicines.
Question 5.2: What is the next thing to tell her?
A. Explain how her chemotherapy works and why she is experiencing this effect?
B. Tell her its alright to refuse chemotherapy.
C. Tell her this is only the first time and it will stop.
D. Tell her “this is not going to stop any time soon.
E. Explain the her family physician can change her chemotherapy.
Click to see the answer
Answer: A
This is a situation where a pharmacist is expected to show empathy. Empathy means the ability to understand another person’s pain and suffering. Note that empathy and sympathy are different. Sympathy means that you feel sorry for another person’s pain.
Question 6: Mechanism of action of Omalizumab
A. TNF Alpha inhibitor
B. Humanized monoclonal antibody
C. B cell depletion
D. HER2 directed analogue of Trustuzumab
E. Inhibits the binding of IgE
Click to see the answer
Answer: E
IgE binds to IgE receptors (Fc epsilon RI receptors = FCERI) and release mediators of allergic response. Omalizumab binds to free IgE, which lowers free IgE levels and cause FCERI receptors on mast cells and basophils. This reduces the release of mediators of allergic response.
Tip: Omalizumab, Mepolizumab, Reslizumab = use in Asthma
Mnemonic 1: Omar Mop the floor and Rest
Mnemonic 2: R-O-Me (ROME) = Reslizumab, Omalizumab, Mepolizumab
| Omalizumab | Mepolizumab | Reslizumab | |
| M (Mechanism) | Anti IgE | Anti IL-5 | Anti IL-5 |
| R (Reduces) | Reduces IgE binding | Reduces Eosinophils | Reduces Eosinophils |
| M (Main use) | Asthma (allergic) | Asthma (Eosinophilic) | Asthma (Eosinophilic) |
Question 7: What is the mechanism of action of Rituximab?
A. TNF Alpha inhibitor
B. B cell depletion with CD80 target site
C. B cell depletion with CD20 target site
D. HER2 inhibitory analogue of Niratinib
E. Inhibits the binding of IgE
Click to see the answer
Answer: C
Rituximab targets CD20 – protein present on all B cells from the stage of cell development. Rituximab binds to this protein (CD20) present on both normal and malignant B-cells. Then, the body’s natural immune defenses are recruited to attack and kill the marked B-cells. Stem cells (young cells in bone marrow) do not have CD20 antigen. Hence, Rituximab is less likely to cause bone marrow suppression.
Rituximab is used in non-Hodgkin’s lymphoma
Question 8: JT is a hypertensive male taking Lisinopril for more than 5 years. Currently, he is complaining that he is not able to sleep properly as he has to wake up in the night a couple of times to urinate. JT is also taking Finasteride for Benign Prostatic Hyperplasia. The doctor prescribed him Alfuzosin. What is the pharmacist’s concern with the prescription?
A. Do not dispense as this is duplication of therapy.
B. No rpoblem to dispense as Alfuzosin is approved for urinary retention in Benign Prostatic Hyperplasia.
C. Do not dispense as JT's sleep disturbances can be managed by dimenhydrinate.
D. Call the doctor and ask to change Alfuzosin with Nifedipine XL as it has better hypertensive control than Alfuzosin.
E. Prazosin is a better option in JT's case as it causes less syncope.
Click here to see the answer
Answer: B
Alfuzosin is approved for urinary retention and symptomatic treatment in Benign Prostatic Hyperplasia. Tamsulosin and Sildosin are α-1A selective blockers.
Prazosin is used for nightmares and scorpion bites.
α-1 blockers/antagonists: 1st gen = Prazosin; 2nd gen = Terazosin, Doxazosin; 3rd gen = Alfuzosin, Sildosin, Tamsulosin. Mnemonic: Post Traumatic Disorder in American Special Troops.
Question 9: KT is a young woman who recently gave birth to a child. She came to the pharmacy to find out if she could store breast milk in the fridge and feed the same milk to the baby during the day when the baby is hungry. What is the pharmacist’s recommendation?
A. should be consumed right away as breast milk cannot be stored at room temperature.
B. Breast Milk can be stored for 24 hours in a cooler with ice packs.
C. Breast milk should never be stored under frozen conditions as it destroys some fo the milk's properties.
D. Pharmacist cannot answer this question and KT should ask her doctor.
E. Can be stored at room temperature upto 25 °C or less for more than 4 hours.
Click here to see the answer
Answer: B
Please remember the below-mentioned information as it is important from PEBC evaluating exam perspective.
| Freshly expressed breast milk | Thawed breast milk (previously frozen) | |
| Room Temperature (25 °C or colder) | Upto 4 Hours | Do not store, Throw away |
| Cooler with Ice packs | Upto 24 Hours | Do not store, Throw away |
| Single door refrigerator (3.8 °C or below) | Upto 3 days | Upto 24 hours |
| In a freezer with a separate door (-17.8 °C or below) | Upto 6 months | Never refreeze thawed milk |
| Single-door refrigerator (3.8 °C or below) | Upto 12 months | Never refreeze thawed milk |
Points to remember:
- Do not use hot water or a microwave to thaw breast milk as it can destroy some of the milk’s properties. Also, it creates hot spots which may cause burn injuries to the baby.
- Never refreeze breast milk.
- When thawing, fat will rise to the top of the milk. Gently stir. Do not shake.
- Use within 1 hour after warming. Discard the remaining if you cannot finish it.
- Always store breast milk at the back of the refrigerator where it is the coldest.
- Store milk in small increments of 2 to 4 oz for easy thawing.
Question 10: What is the preferred anticoagulant for a patient who has stage 5 renal disease?
A. Abciximab
B. Dabigatran
C. Rivaroxaban
D. Enoxaparin
E. Warfarin
Click here to see the answer
Answer: E
Warfarin has 100% hepatic elimination. Hence, Warfarin is the answer.
Question 11: What is the mechanism of action of Finasteride?
A. Xanthine Oxidase inhibitor
B. Competitive and specific inhibition of 5-α reductase type II.
C. Pseudo irreversible inhibition of 5-α reductase type II.
D. Stimulates the conversion of Testosterone to dehydroxy testosterone by acting as an agonist of 5-α reductase type II.
E. Competitive and specific inhibition of 5-α reductase type I.
Click here to see the answer
Answer: B
Notes for quick revision:
- 5-α reductase inhibitors:
- Finasteride (inhibition of 5-α reductase type II)
- Used in BPH and male alopecia
- Dutasteride (inhibition of 5-α reductase type I and type II)
- Finasteride (inhibition of 5-α reductase type II)
- Side effects: Decreased libido and sexual dysfunction, hypersensitive reactions like rash and testicular pain.
- Contraindication: Not indicated for use in women and children.
Question 12: Which is the important invivo factor for the disintegration of oral solid dosage forms?
A. Gastric peristalysis helps with the breaking of tablets and capsules.
B. Gastrin secreted by G cells of the stomach.
C. Amylase and Lipase found in the stomach.
D. Gastric acidic pH is the most contributing factor.
E. Use of a superdisintegrant like sodium starch glycollate.
Click here to see the answer
Answer: D
Explanation:
Peristalsis moves the content of the stomach to the intestine. It has no role in disintegration as such. None of the enzymes found in the stomach do not play a major role in disintegration. Since the question is asking for invivo factor, we can rule out super disintegrants as it is not invivo.
Question 13: A patient was prescribed Drug X, administered orally at a dosage of 250 mg every 8 hours. The bioavailability of the drug is 1 (100%), and its clearance rate is 2.8 ml/hr. What is the steady-state concentration of Drug X in the patient?
A. 11.16 mg/ml
B. 12.52 mg/ml
C. 15.83 mg/ml
D. 18.39 mg/ml
E. 20.17 mg/ml
Click here to see the answer
Answer: A
Explanation:
Css = F×D / cl×t where F bioavailability D dose Cl clearance T interval
Css = 1 x 250 / 2.8 x 8 = 11.16 mg/ml
Question 14: JT is a 54-year-old male taking Metformin and Amiodarone. His hemoglobin is decreased and he has a high mean cell volume (MCV). What is the cause of his anemia?
A. Iron deficiency
B. Chronic disease
C. Vitamin B12 deficiency
D. Folate deficiency
E. Thalassemia
Click here to see the answer
Answer: C
Question 15: Which of the following is needed to absorb vitamin B12?
A. Iron
B. Zinc
C. Intrinsic factor
D. Magnesium
E. Calcium
Click here to see the answer
Answer: C
Question 16: A patient is taking oral contraceptives and she always starts her medication on Sunday, she forgot to take two doses in the second week, what should you told her to do:
A. Discard the strip and begin with another one
B. Take the daily tablet until the next Sunday and start a new strip
C. Take two tablets today, then two tablets tomorrow and then continue the strip
D. Safely continue the strip without warring
E. Talk to the doctor
Click here to see the answer
Answer: C
Question 17: Which of the following increase with age?
A‐ Parathyroid hormone
B- Total body water
C- Bone mass
D- Hair growth
E- Clearance
Click here to see the answer
Answer: C
Parathyroid hormone decreases with age due to a decline in renal function.
Question 18: Which of the following is the most suitable corticosteroid for diaper rash?
A. 0.025 % hydrocortisone
B. 0.5% hydrocortisone
C. 0,05 % betamethasone
D. Acetamide 0.05%
E. Hydrocortisone 2%
Click here to see the answer
Answer: C
Hydrocortisone up to 1% is OTC
Question 19: What is the mechanism of action of Dorzolamide?
A. Decreases the production of aqueous humor
B. Increases the outflow of aqueous humor
C. Decreases the production of vitreous humor
D. Increases the outflow of vitreous humor
E. Both A and B
Click here to see the answer
Answer: A
Dorzolamide is a carbonic anhydrase inhibitor that decreases the production of aqueous humor.
Question 20: Which of the following is the rate-controlling membrane for ophthalmic dosage forms?
A. Cornea
B. Pupil
C. Lens
D. Iris
E. Macula
Click here to see the answer
Answer: A
Cornea is the outermost layer and the rate controlling membrane.
Question 21: Which of the following is a side effect of Isoniazid?
A. Dermatitis
B. Stevens Johnson Syndrome
C. Systemic Lupus Erythematous
D. Peripheral neuropathy
E. Diarrhea
Click here to see the answer
Answer: D
This is due to deficiency of vitamin B6. Because of this deficiency, it reduces seizure threshold in these patients. So, if they get a seizure, even Diazepam might be ineffective. If these patients are given B6, it will also help them with their seizure.
Question 22: A woman is taking oral contraceptives. Which of the following should be monitored after 4 weeks?
A. Calcium
B. Potassium
C. Sodium
D. Chloride
E. Magnesium
Click here to see the answer
Answer: B
Question 23: Which of the following can a pharmacy assistant can do?
A. Enter a new prescription into software
B. Check the prescription is authentic and right
C. Take oral prescriptions for narcotics
D. Advice about OTC products
E. Check drug - disease compatibility of the prescription
Click here to see the answer
Answer: A
Question 24: Which of the following is a source of calcium for muscle contraction?
A. Kidney
B. Intestine
C. Extracellular
D. Intracellular
E. Diet
Click here to see the answer
Answer: C
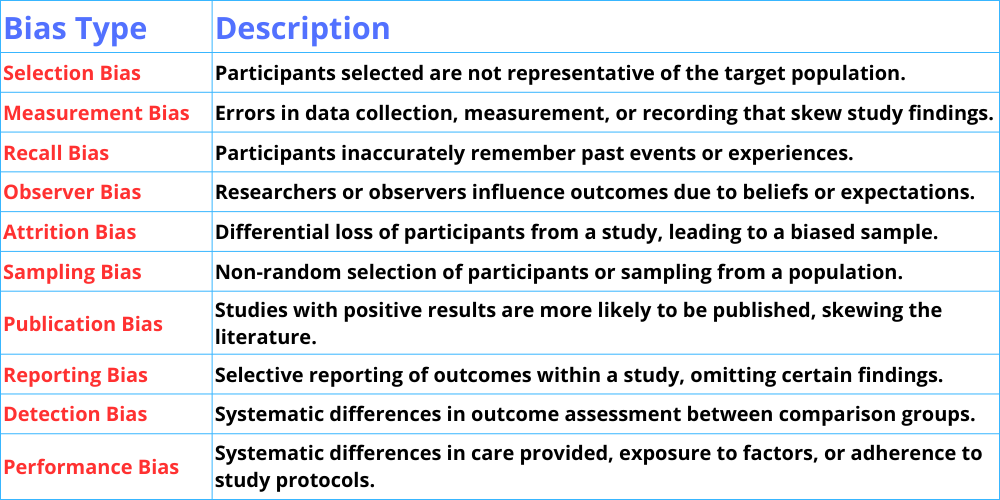
Question 25: Which of the following in a study will lead to bias?
A. Low sample size
B. Blinding of the sponsor
C. Blinding of the investigator
D. Random selection of population
E. Asking the subjects to select their own group
Question 26: JT, a 68-year-old male, presents with frequent nighttime urination, difficulty initiating and maintaining urine flow, and occasional post-void dribbling. He has a history of hypertension and is on daily medication. A digital rectal examination shows an enlarged prostate gland. JT is prescribed Ramipril, Finasteride, and Terazosin. Answer the following questions based on the given information
Question 26.1: What do you think about the prescription?
A. Suitable therapy
B. Duplication of therapy
C. Drug-disease contraindication
D. Drug-drug contraindication
E. Therapy not suitable die to side effects
Click here to see the answer
Answer: A
Question 26.2: Which of the following drugs is contraindicated with JT’s medication profile?
A. Testosterone
B. Sildenafil
C. Nitorglycerine
D. Furosemide
E. Nifedipine XL
Click here to see the answer
Answer: A
Finasteride and testosterone have opposite effects.
Question 27: A 17-year-old girl comes to the pharmacy with complaints of pain and discharge from her ear. She is on a swimming course. What’s the most likely to be the cause?
A. Otitis media
B. Otitis externa
C. Chronic bronchitis
D. Allergic rhinitis
E. Migrane
Click here to see the answer
Answer: B
Cause of otitis external – Pseudomonas aeruginosa
Question 28: Which of the following drugs causes the least hypoglycemia?
A- Gliclazide
B- Glimepiride
C- Glyburide
D‐ Sitagliptin
E- Repaglinide
Click here to see the answer
Answer: D
Question 29: Which of the following is the correct statement for bacterial vaginosis?
A. Thick, white discharge with a cottage cheese consistency, accompanied by itching and burning in the vulvar area.
B. Greenish-yellow, frothy discharge causing discomfort when urinating (dysuria).
C. Heavy discharge with blood streaks and pelvic pain.
D. Thin, grayish discharge with a fishy odor, especially noticeable after sexual intercourse.
E. Limited discharge accompanied by vaginal dryness and burning.
Question 30: In the human body, what is the primary source of the nitrogen atom found in nitric oxide (NO)?
A. L-Arginine
B. Alanine
C. Leucine
D. Glutamine
E. Aspartate
Click here to see the answer
Answer: A
Question 31: You are working as a pharmacist in a community pharmacy. A patient who may identify differently from their previous records visits your pharmacy for the first time. How should your staff prioritize creating a welcoming environment?
A. Rely solely on information in the system, regardless of the patient's current preferences.
B. Use labels based on assumptions about the patient's background.
C. Ask the patient how they prefer to be addressed.
D. Avoid discussing pronouns altogether until the patient initiates the conversation.
E. Use exclusively gender-neutral language without acknowledging the context.
Click here to see the answer
Answer: C
Explanation
- Firstly – Ask the patient how would they like to be addressed. [This is because ‘ask’, do not assume]
- Alternatively – If the patient is uncomfortable addressing this issue, use gender-neutral pronouns
Question 32: JT, a 29-year-old female is experiencing gastrointestinal (GIT) side effects from her prescribed Erythromycin. You, the pharmacist, are calling the physician to discuss treatment options. What is the MOST appropriate and professional way to initiate the conversation?
A. I am sorry to disturb you, do you have time to discuss JT's case?
B. Are you aware that Erythromycin that u prescribed caused GIT side effects to JT?
C. I am calling about JT. She claims she can't take her medication because she can't tolerate the GIT SEs, how about considering Azithromycin?
D. Report that a patient is experiencing problems with Erythromycin and request next steps.
E. Instruct the doctor to switch JT to Azithromycin for stomach issues.
Click here to see the answer
Answer: C
Explanation: Let’s analyze each option one by one.
A – Here you are asking the doctor if he has the time to discuss. What if the doctor says that he does not have time. Will you keep the patient waiting or will you deny the patient to provide care and professional service? – So, this is not the right option.
B – Here, you are asking the doctor if he is aware of the patient’s side effects. Since the patient came to the pharmacy, it implies that JT did not go to consult the doctor and hence the doctor is unaware. Also, the tone of this statement is accusatory. – So this is not the right option.
C – Right answer because the tone is polite and you (the pharmacist) is not accusing or questioning the doctor’s judgment. Also, your conversation is to the point which reflects that you value your time as well as the doctor’s time.
D – This option is similar to C, but it lacks a suggestion. You as a pharmacist should be providing your professional judgment.
E – As a pharmacist, you can give your professional opinion to the doctor, but you cannot give instructions to other healthcare provider unless the actions of other provider may cause harm to the patient. – So, this is not the right option.
Join Our Facebook Group
Questions posted every day to help you succeed.
PEBC Evaluating Exam Preparation